Respiratory system
The respiratory system stands as both conductor and performer, orchestrating the delicate dance of breath. From the first inhalation at birth to the final exhalation that marks our earthly journey’s end, our lungs tirelessly exchange gases, ensuring our survival. In this article, we embark on a voyage through the winding airways, exploring the anatomy, function, and remarkable collaboration of the respiratory system with other bodily systems.
Anatomy of respiratory system
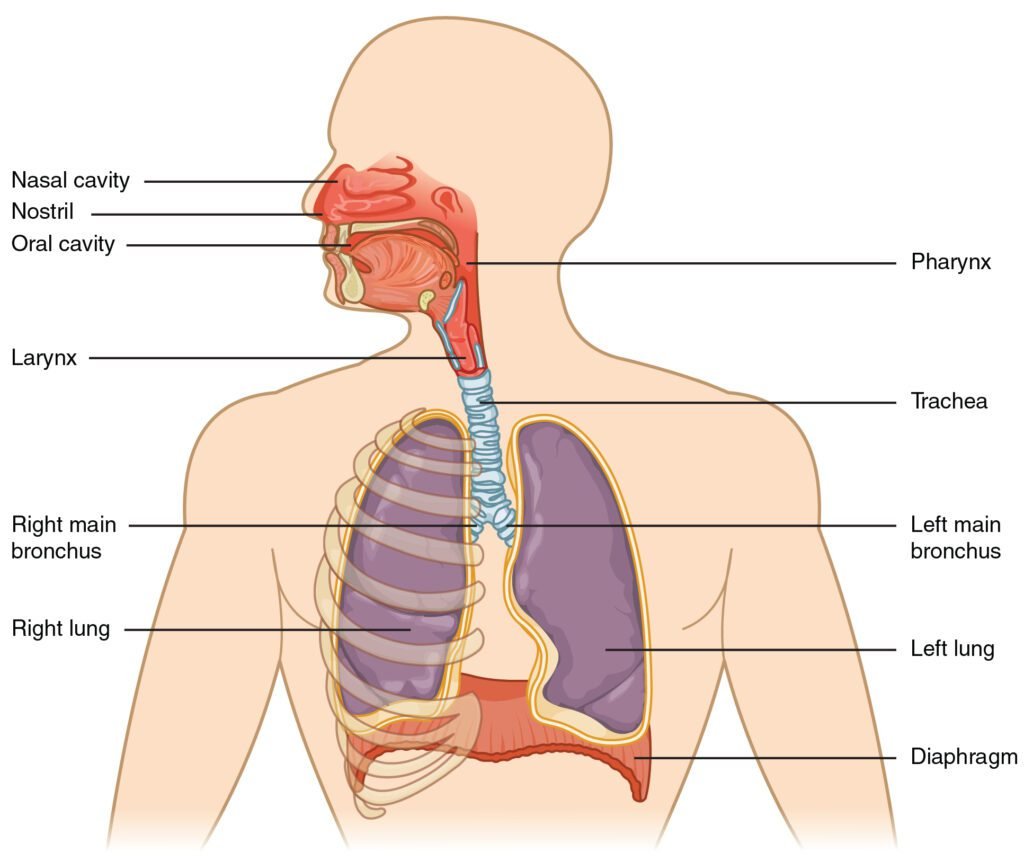
Major Organs
- Lungs: The stars of the show! These spongy, air-filled structures reside within the chest cavity and perform gas exchange.
- Nose and Nasal Cavity: The entry point for air. The nose filters, warms, and humidifies incoming air.
- Mouth and Oral Cavity: An alternate route for air intake.
- Pharynx (Throat): The junction where the nasal and oral passages meet.
- Larynx (Voice Box): Houses the vocal cords and allows us to speak.
- Trachea (Windpipe): A sturdy tube connecting the larynx to the bronchi.
- Bronchi (Large Airways): These branch into smaller bronchioles, leading to the lungs.
- Diaphragm: The superstar muscle responsible for breathing. It contracts during inhalation and relaxes during exhalation.
Minor Organs and Structures
- Paranasal Sinuses: Air-filled cavities in the skull that contribute to air conditioning and resonance.
- Sinuses: These spaces around the nasal cavity also play a role in air conditioning.
- Bronchioles: Tiny airways branching from the bronchi, further dividing into alveolar ducts.
- Alveoli: The real MVPs! These microscopic air sacs within the lungs facilitate gas exchange with blood vessels.
- Blood Vessels: The pulmonary arteries and veins transport oxygenated and deoxygenated blood to and from the lungs.
- Ribs: Not organs per se, but they protect the respiratory system like loyal guardians.
Upper Respiratory Tract vs. Lower Respiratory Tract
- Upper Respiratory Tract: Includes the nasal cavity, paranasal sinuses, pharynx, and the portion of the larynx above the vocal cords.
- Lower Respiratory Tract: Encompasses the larynx below the vocal cords, trachea, bronchi, bronchioles, and the lungs.
Upper respiratory tract
Nose and Nasal Cavity
- The nose serves as our primary entry point for air.
- Nostrils (nares) create openings to the outside world.
Inside the nasal cavity
- Nasal conchae (turbinates): Scroll-shaped bones that swirl the air, allowing time for humidification, warming, and cleaning.
- Epithelial cilia: These tiny hairlike structures, along with mucous membranes, trap unwanted particles.
- The filtered, warmed air exits the nasal cavities into the nasopharynx, the uppermost part of the pharynx.
Paranasal Sinuses
- These are four paired, air-filled cavities within skull bones (frontal, ethmoidal, sphenoidal, and maxillary sinuses).
- Mucosae lining the sinuses help warm and humidify inhaled air.
- Mucus drains from the sinuses into the nasal cavities.
Pharynx (Throat): Shaped like a funnel, the pharynx connects various regions;
- Nasopharynx: Posterior to the nasal cavity, it serves as an air passageway.
- Oropharynx: Posterior to the oral cavity, it contains the palatine tonsils and allows both air and ingested food to pass.
- Laryngopharynx: Lies below the epiglottis, connecting to the larynx (superiorly) and the esophagus (inferiorly). During breathing, the epiglottis stays up, allowing free airflow.
Larynx (Voice Box)
- Connects the lower part of the pharynx (laryngopharynx) to the trachea.
Key functions
- Keeps air passages open during breathing and digestion.
- Produces sound (phonation) via movement of air across the vocal cords.
- Comprised of nine cartilages, including the lifesaving epiglottis (which prevents food from entering the airway during swallowing).
Lower respiratory tract
Trachea (Windpipe)
- The trachea is a tube less than an inch in diameter, covered by cartilaginous rings.
- It extends from the bottom of the larynx down behind the sternum, where it branches into smaller tubes called bronchi.
- During inhalation, air filtered and warmed by the upper respiratory system passes from the pharynx and larynx into the trachea, then down to the bronchi and into the lungs.
- Deoxygenated air from the lungs passes back up through the trachea during exhalation.
- The cartilaginous rings support the trachea, preventing it from over-expanding or collapsing (similar to how a straw stays open when you suck on it). These rings are C-shaped, with a gap on the posterior side, allowing the trachea to bend when the esophagus presses against it during swallowing.
Bronchi and Bronchioles
- The tubes of the primary bronchi branch off from the bottom of the trachea.
- These branches further divide into secondary and tertiary bronchi, which then become smaller and smaller, forming the bronchioles.
- These progressively smaller airways deliver oxygen-rich air from the trachea to the lungs.
- During exhalation, deoxygenated air (now rich with carbon dioxide) leaves the lungs by the reverse route.
- When we exercise, relaxation of smooth muscle in the bronchioles causes them to dilate, allowing greater ventilation. Conversely, allergic reactions and histamines cause the opposite effect—bronchoconstriction.
Alveoli and External Respiration
- Alveoli are microscopic air sacs served by the bronchioles.
- They are the sites of external respiration.
- Oxygen diffuses from the alveoli into the bloodstream, while carbon dioxide diffuses from the capillaries into the alveoli.
- This exchange ensures that our cells receive oxygen and dispose of carbon dioxide.
Anatomy of lungs

Position and Relations
- The lungs lie on either side of the mediastinum within the thoracic cavity.
- Each lung is surrounded by a pleural cavity, formed by the visceral and parietal pleura.
- The lungs are suspended from the mediastinum by the lung root, a collection of structures entering and leaving the lungs.
- Medial surfaces of both lungs are close to several mediastinal structures:
Left Lung
- Heart
- Arch of aorta
- Oesophagus
- Inferior vena cava
Right Lung
- Heart
- Thoracic aorta
- Oesophagus
- Superior vena cava
- Azygous vein
Lung Structure: Each lung consists of;
- Apex: The blunt superior end projecting above the level of the 1st rib into the neck.
- Base: The inferior surface resting on the diaphragm.
- Lobes (two or three)
- Separated by fissures within the lung.
- The right lung has three lobes (superior, middle, and inferior).
- The left lung has two lobes (superior and inferior).
Surfaces (three)
- Costal: Facing the ribs.
- Mediastinal: Facing the mediastinum.
- Diaphragmatic: Resting on the diaphragm.
Borders (three)
- Anterior: The edge facing forward.
- Inferior: The lower edge.
- Posterior: The edge against the vertebral column.
Alveoli and Gas Exchange
- Alveoli are microscopic air sacs within the lungs.
- Oxygen diffuses from the alveoli into surrounding capillaries, while carbon dioxide diffuses in the opposite direction.
- This exchange ensures that our cells receive oxygen and dispose of carbon dioxide.
Mechanism of respiration
- Breathing Mechanism (Pulmonary Ventilation)
- Breathing, also known as pulmonary ventilation, involves the movement of air in and out of the lungs.
- The air we inhale and exhale follows a specific pathway;
Inhalation (Inspiration)
Muscles Involved
- Diaphragm: A dome-shaped muscle below the lungs.
- External Intercostal Muscles: Muscles between the ribs.
Process
- During inhalation, the diaphragm contracts and moves downward, expanding the chest cavity vertically.
- The external intercostal muscles contract, lifting the ribcage and expanding the chest cavity horizontally.
- These combined actions increase the volume of the thoracic cavity, creating a partial vacuum.
- Air rushes into the lungs through the trachea and bronchi, filling the alveoli.
Exhalation (Expiration)
Muscles Involved
- Internal Intercostal Muscles: Muscles between the ribs.
- Abdominal Muscles: Muscles of the abdominal wall.
Process
- During exhalation, the diaphragm relaxes and moves upward, reducing the chest cavity volume.
- The internal intercostal muscles contract, pulling the ribcage downward.
- The abdominal muscles contract, pushing the diaphragm further up.
- These actions increase the pressure in the thoracic cavity, forcing air out of the lungs.
Gas Exchange (External Respiration)
- The actual exchange of gases occurs in the alveoli (tiny air sacs within the lungs).
- Oxygen from the inhaled air diffuses into the capillaries surrounding the alveoli, binding to hemoglobin in red blood cells.
- Carbon dioxide, a waste product, diffuses from the capillaries into the alveoli to be exhaled.
Control of Breathing
- Breathing is regulated by the respiratory centers in the brainstem (medulla oblongata and pons).
- These centers monitor blood pH, oxygen, and carbon dioxide levels.
- Signals from chemoreceptors adjust the breathing rate and depth to maintain homeostasis.
Regulation of respiration
Central Control Centers: The brainstem houses the primary respiratory centers;
Medulla Oblongata
- Contains the dorsal respiratory group (DRG) and the ventral respiratory group (VRG).
- The DRG initiates and controls the basic rhythm of breathing.
- The VRG is involved in forced breathing (e.g., during exercise).
Pons
- Contains the pneumotaxic center and the apneustic center.
- The pneumotaxic center fine-tunes the breathing rate by inhibiting the DRG.
- The apneustic center stimulates the DRG, prolonging inhalation.
Chemoreceptors
Central Chemoreceptors
- Located in the medulla.
- Sensitive to changes in cerebrospinal fluid (CSF) pH due to carbon dioxide levels.
- High CO₂ levels lead to increased ventilation.
Peripheral Chemoreceptors
- Located in the carotid bodies (near carotid arteries) and aortic bodies (near aortic arch).
- Sensitive to changes in arterial blood pH, CO₂, and oxygen levels.
- High CO₂ or low oxygen triggers increased ventilation.
Feedback Mechanisms
Negative Feedback
- High CO₂ or low oxygen levels stimulate chemoreceptors.
- The brainstem adjusts ventilation rate to restore homeostasis.
Positive Feedback
- During intense exercise, feedback mechanisms override normal regulation.
- Increased ventilation leads to more oxygen uptake and CO₂ removal.
Other Factors
Lung Stretch Receptors
- Located in the bronchi and bronchioles.
- Inhibit inspiration if lung tissue is overstretched.
Irritant Receptors
- Detect noxious substances (e.g., smoke, dust) in airways.
- Trigger coughing or sneezing reflexes.
Lung volume
Lung volumes refer to the different amounts of air that can be inhaled, exhaled, or remain in the lungs during various phases of breathing. These volumes are crucial for assessing lung health and function. Let’s break them down:
Tidal Volume (TV)
- Tidal volume is the volume of air inhaled or exhaled during a normal, quiet breath.
- It represents the amount of air that moves in and out with each breath.
- On average, tidal volume is about 500 milliliters (ml).
Inspiratory Reserve Volume (IRV)
- IRV is the additional volume of air that can be forcibly inhaled after a normal inhalation.
- It represents the extra air you can take in during a deep breath.
- On average, IRV is about 2,500 ml.
Expiratory Reserve Volume (ERV)
- ERV is the additional volume of air that can be forcibly exhaled after a normal exhalation.
- It represents the extra air you can expel during a forceful breath out.
- On average, ERV is about 1,500 ml.
Residual Volume (RV)
- RV is the volume of air that remains in the lungs after maximum exhalation.
- It cannot be measured directly using spirometry.
- RV ensures that the alveoli stay open and prevents lung collapse.
- On average, RV is about 1,500 ml.
Lung Capacities
Lung capacities are combinations of two or more lung volumes. They provide a broader perspective on lung function. Let’s explore them:
Vital Capacity (VC) or Forced Vital Capacity (FVC)
- Vital capacity is the maximum volume of air that can be exhaled after a maximum inhalation.
- It includes the tidal volume, inspiratory reserve volume, and expiratory reserve volume.
- VC reflects lung compliance, muscle strength, and airway resistance.
- On average, vital capacity is about 4,500 ml.
Inspiratory Capacity (IC)
- Inspiratory capacity is the volume of air that can be inhaled from a normal exhalation.
- It includes the tidal volume and inspiratory reserve volume.
- IC represents the maximum amount of air you can breathe in.
- On average, inspiratory capacity is about 3,000 ml.
Functional Residual Capacity (FRC)
- FRC is the volume of air remaining in the lungs after a normal exhalation.
- It includes the expiratory reserve volume and residual volume.
- FRC ensures that the lungs stay partially inflated.
- On average, functional residual capacity is about 3,000 ml.
Total Lung Capacity (TLC)
- Total lung capacity is the maximum volume of air the lungs can hold.
- It includes all lung volumes: tidal volume, inspiratory reserve volume, expiratory reserve volume, and residual volume.
- TLC reflects lung size and compliance.
- On average, total lung capacity is about 6,000 ml.
Transport of Respiratory Gases
Oxygen (O₂)
- Oxygen diffuses from the alveoli into the bloodstream.
- It binds to hemoglobin in red blood cells, forming oxyhemoglobin.
- Oxyhemoglobin is transported to body tissues, where oxygen is released for cellular respiration.
Carbon Dioxide (CO₂)
- Carbon dioxide is produced during cellular respiration.
- It diffuses from body tissues into the bloodstream.
- In the blood, CO₂ combines with water to form carbonic acid (H₂CO₃).
- Carbonic acid dissociates into bicarbonate ions (HCO₃⁻) and hydrogen ions (H⁺).
- Bicarbonate ions are transported back to the lungs, where they combine with hydrogen ions to form carbonic acid.
- Carbonic acid dissociates back into CO₂ and water, which are exhaled from the lungs.
Artificial respiration
This life-saving technique is crucial when natural respiration has ceased or is faltering. By applying specific manipulative techniques, we can prevent deaths from drowning, choking, strangulation, suffocation, carbon monoxide poisoning, and electric shock. Let’s explore the details:
What Is Artificial Respiration?
- Artificial respiration refers to breathing induced by some manipulative technique when natural respiration is compromised.
- The goal is to maintain oxygen supply and remove carbon dioxide from the body.
- Properly applied artificial respiration can prevent fatalities in critical situations.
Methods of Artificial Respiration
Mouth-to-Mouth Breathing (Rescue Breathing): This method involves direct contact between the rescuer and the victim.
Steps
- Place the victim on their back.
- Clear the mouth of foreign material and mucus.
- Lift the lower jaw forward and upward to open the air passage.
- Create a leak-proof seal by placing your mouth over the victim’s mouth.
- Clamp the victim’s nostrils.
- Deliver rescue breaths (exhalations) into the victim’s mouth.
- Observe chest rise and fall.
- Repeat at a rate of about 10–12 breaths per minute.
- Mouth-to-mouth breathing is effective and widely used.
Mouth-to-Nose Breathing
- Similar to mouth-to-mouth, but the rescuer seals the victim’s nose instead of the mouth.
- Useful when the victim has a mouth injury or obstruction.
Mouth-to-Stoma Breathing
- Used for individuals with a tracheostomy (stoma) tube.
- Seal the stoma and deliver rescue breaths.
Bag-Valve-Mask (BVM) Ventilation
- A manual resuscitator device with a self-expanding bag, one-way valve, and mask.
- Used by healthcare professionals.
- Provides positive pressure ventilation to the victim.
- Requires proper training to avoid complications.
Mechanical Ventilation (Ventilators)
- Used in hospitals and critical care settings.
- Mechanical ventilators deliver controlled and synchronized breaths to patients.
- Various modes are available based on the patient’s condition.
When to Use Artificial Respiration
- Drowning: Victims pulled from water need immediate artificial respiration.
- Choking: If the Heimlich maneuver fails, artificial respiration is crucial.
- Carbon Monoxide Poisoning: Administer oxygen and provide artificial respiration.
- Electric Shock: Victims may stop breathing due to muscle paralysis.
- Suffocation: Victims trapped in confined spaces or under debris require prompt intervention.
Artificial respiration and resuscitation methods are related but distinct techniques used in emergency situations.
Artificial Respiration
Purpose
- Artificial respiration is necessary when natural breathing has stopped or is insufficient.
- It aims to maintain an open airway and facilitate gas exchange in the lungs.
Methods
- Mouth-to-mouth breathing (rescue breathing) is a common form of artificial respiration.
- Other methods include mouth-to-nose breathing and mouth-to-stoma breathing (for tracheostomy patients).
Goal
- To provide oxygen and remove carbon dioxide until the victim can breathe independently.
Resuscitation Methods
Purpose
- Resuscitation methods aim to restore circulation and breathing in life-threatening situations.
- They include both artificial respiration and other interventions.
Components
- CPR (cardiopulmonary resuscitation) combines chest compressions and rescue breaths.
- AED (automated external defibrillator) delivers electric shocks to restore normal heart rhythm.
- ALS (advanced life support) involves advanced airway management, medications, and defibrillation.
Application
- Resuscitation methods are used during cardiac arrest, drowning, choking, and other critical emergencies.
Collaboration with other systems
Collaboration with the Circulatory System (Cardiovascular System)
Gas Exchange
- The primary collaboration occurs in the alveoli of the lungs.
- Oxygen (O₂) diffuses from the alveoli into the capillaries surrounding them.
- Oxygen binds to hemoglobin in red blood cells, forming oxyhemoglobin.
- Oxyhemoglobin is transported via blood vessels to body tissues for cellular respiration.
- Carbon dioxide (CO₂), a waste product, diffuses from tissues into capillaries and is carried back to the lungs.
- In the lungs, CO₂ is released into the alveoli for exhalation.
pH Regulation
- The respiratory system helps regulate blood pH by controlling CO₂ levels.
- High CO₂ leads to acidosis, while low CO₂ leads to alkalosis.
- Chemoreceptors in the brainstem monitor CO₂ levels and adjust ventilation accordingly.
Blood Pressure Regulation
- The respiratory system influences blood pressure through oxygen and CO₂ levels.
- Proper oxygenation helps maintain blood vessel tone and overall cardiovascular health.
Collaboration with the Skeletal System: Rib Cage and Diaphragm;
- The rib cage protects the lungs and provides structural support.
- During inhalation, the rib cage expands, increasing lung volume.
- The diaphragm, a dome-shaped muscle below the lungs, contracts during inhalation.
- These movements facilitate breathing.
Collaboration with the Nervous System: Medulla Oblongata;
- The medulla contains the respiratory centers that regulate breathing.
- These centers monitor blood pH, oxygen, and CO₂ levels.
- Signals from chemoreceptors adjust breathing rate and depth.
Cough Reflex and Sneezing
- The nervous system triggers protective reflexes to clear airways.
- Coughing removes irritants, while sneezing expels foreign particles.
Collaboration with the Integumentary System: Skin and Sweat Glands;
- The skin helps regulate body temperature.
- Sweating cools the body during increased respiratory effort (e.g., exercise).
Common disorders
Asthma
- Description: Asthma is a chronic inflammatory disease that affects the airways.
- Causes: Genetic factors, environmental triggers (allergens, smoke, pollution), and respiratory infections.
Symptoms
- Wheezing
- Coughing (especially at night or early morning)
- Shortness of breath
- Chest tightness
Treatment
- Inhalers (bronchodilators and anti-inflammatory medications)
- Avoiding triggers
- Allergy management
Chronic Obstructive Pulmonary Disease (COPD)
- Description: COPD is an umbrella term for two primary obstructive lung diseases: emphysema and chronic bronchitis.
- Causes: Smoking, exposure to pollutants
- Pathophysiology: Damage to alveoli (air sacs), leading to reduced gas exchange
Symptoms
- Shortness of breath
- Chronic cough
- Barrel chest (due to lung hyperinflation)
Treatment
- Smoking cessation
- Bronchodilators
- Oxygen therapy
Chronic Bronchitis
- Causes: Smoking, air pollution
- Pathophysiology: Inflammation of bronchial tubes, excessive mucus production
Symptoms
- Persistent cough with mucus
- Shortness of breath
- Frequent respiratory infections
Treatment
- Bronchodilators
- Mucolytics
- Pulmonary rehabilitation
Cystic Fibrosis
- Description: A genetic disorder affecting the respiratory and digestive systems.
- Causes: Inherited gene mutations (autosomal recessive)
- Pathophysiology: Defective chloride transport leads to thick, sticky mucus production. Mucus clogs airways, causing recurrent infections and lung damage.
Symptoms
- Chronic cough
- Frequent lung infections
- Difficulty gaining weight
Treatment
- Chest physiotherapy
- Enzyme replacement therapy
- Antibiotics
Lung Cancer
- Description: Uncontrolled growth of abnormal cells in the lungs.
- Causes: Smoking, exposure to carcinogens (asbestos, radon)
Symptoms
- Persistent cough
- Hemoptysis (coughing up blood)
- Chest pain
- Weight loss
Treatment
- Surgery
- Radiation
- Chemotherapy
Tuberculosis (TB)
- Description: Infectious disease caused by Mycobacterium tuberculosis.
- Transmission: Airborne droplets
Symptoms
- Chronic cough
- Night sweats
- Weight loss
- Fatigue
Treatment
- Antibiotics (long-term therapy)
Bronchitis
- Description: Inflammation of the bronchial tubes.
Acute Bronchitis:
- Usually caused by viral infections
- Self-limiting
- Symptoms: Cough, mucus production
Chronic Bronchitis
- Persistent inflammation
- Part of COPD
- Symptoms: Chronic cough, shortness of breath
Pneumonia
- Description: Infection of lung tissue (alveoli)
- Causes: Bacteria, viruses, fungi
Symptoms
- Fever
- Cough with phlegm
- Chest pain
- Difficulty breathing
Treatment
- Antibiotics (for bacterial pneumonia)
- Rest and hydration
Conclusion
The respiratory system, often taken for granted, is a marvel of intricate design and functionality. From the moment we take our first breath to the countless inhalations that sustain us, this system ensures our survival. Here are the key takeaways:
- Gas Exchange: The lungs, with their millions of alveoli, facilitate the exchange of oxygen and carbon dioxide. Through inspiration and expiration, we maintain the delicate balance necessary for life.
- Collaboration: The respiratory system collaborates seamlessly with other systems. It partners with the circulatory system for oxygen transport, the skeletal system for chest movement, and the nervous system for regulation.
- Common Disorders: Asthma, COPD, lung cancer, and infections challenge our respiratory health. Recognizing symptoms and seeking timely intervention are crucial.
- Life-Saving Techniques: CPR, AEDs, and advanced life support play pivotal roles in emergencies. Knowing when and how to apply them can make all the difference.
For more regular updates you can visit our social media accounts,
Instagram: Follow us
Facebook: Follow us
WhatsApp: Join us
Telegram: Join us