Cardiovascular System
The cardiovascular system, often referred to as the lifeline of the body, is a marvel of biological engineering. This intricate network, comprising the heart, blood vessels, and blood, serves as the body’s primary transportation system. It ensures the delivery of essential nutrients, oxygen, and hormones to every cell, while simultaneously removing waste products and carbon dioxide. Its ceaseless operation, beating approximately 100,000 times a day and pumping nearly 2,000 gallons of blood, is testament to its critical role in our survival and overall health.
Heart
- Location and Structure: The heart is a muscular organ located in the mediastinum, the central compartment of the thoracic cavity. It is situated slightly to the left of the center, behind the breastbone, and rests on the diaphragm. The heart is shaped like a quadrangular pyramid, with its base facing the posterior thoracic wall and its apex pointing towards the anterior thoracic wall.
- Surfaces and Margins: The heart has five surfaces: base (posterior), diaphragmatic (inferior), sternocostal (anterior), and left and right pulmonary surfaces. It also has several margins: right, left, superior, and inferior. The right margin is the small section of the right atrium that extends between the superior and inferior vena cava. The left margin is formed by the left ventricle and left auricle.
- Chambers Inside: The heart is divided into four chambers: two atria (right and left) and two ventricles (right and left). The right atrium and ventricle receive deoxygenated blood from systemic veins and pump it to the lungs, while the left atrium and ventricle receive oxygenated blood from the lungs and pump it to the systemic vessels which distribute it throughout the body.
- Valves: The heart contains four valves: the tricuspid, pulmonary, mitral, and aortic valves. These valves control the flow of blood within the different chambers.
- Blood Supply: The heart’s blood supply comes from the right and left coronary arteries. The right coronary artery has several branches, including the sinuatrial nodal branch, right marginal branch, atrioventricular nodal branch, and posterior interventricular branch. The left coronary artery has the circumflex branch and anterior interventricular branch.
- Pericardium: The heart is wrapped in a two-layered serous sac called the pericardium. This sac protects the heart and anchors it to the surrounding structures.
- Myocardium and Endocardium: The heart consists of several layers of a tough muscular wall, the myocardium. A thin layer of tissue, the pericardium, covers the outside, and another layer, the endocardium, lines the inside.
Blood circulation
Blood circulation, also known as the cardiovascular system, is a complex process that involves the continuous movement of blood throughout the body, driven by the pumping action of the heart.
- Components of the Circulatory System: The circulatory system consists of the heart, blood vessels, and blood. The heart pumps blood, the blood vessels transport it, and the blood carries oxygen, nutrients, and hormones to various parts of the body.
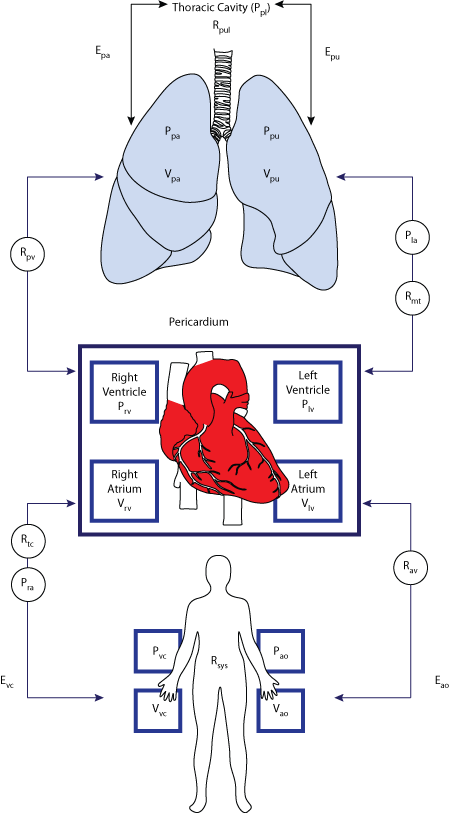
- Circulatory Pathways: The circulatory system has two main pathways: the systemic circulation and the pulmonary circulation.
- Systemic Circulation: This is the part of the circulatory system that carries oxygenated blood from the heart to the rest of the body, and returns deoxygenated blood back to the heart.
- Pulmonary Circulation: This is the part of the circulatory system that carries deoxygenated blood from the heart to the lungs, where it picks up oxygen and releases carbon dioxide. The oxygenated blood then returns to the heart.
- Blood Flow: Blood flows through your heart, lungs, and body in a series of steps. After delivering oxygen and nutrients to all your organs and tissues, your blood enters your heart and flows to your lungs to gain oxygen and get rid of waste. It then flows back to your heart, which pumps the refreshed blood out through your aorta to nourish your body again.
- Role of the Circulatory System: The circulatory system is critical to healthy organs, muscles, and tissues. It links the sites of oxygen utilization and uptake in the body. It also helps the immune system to fight diseases and helps maintain homeostasis by stabilizing temperature and natural pH.
Blood vessels
Blood vessels are an integral part of the circulatory system, serving as the body’s transportation network for blood. There are three main types of blood vessels: arteries, veins, and capillaries.
Arteries
Structure of arteries: Arteries are muscular, elastic tubes that play a crucial role in the circulatory system. The wall of an artery is made up of three layers:
- Tunica Externa (Adventitia): This is the outermost layer of arteries, composed of connective tissue made of collagens and elastic tissues. It provides structural support and allows the arteries to stretch to prevent overexpansion due to the pressure exerted by blood flow.
- Tunica Media: This is the middle layer, primarily composed of smooth muscle fibers arranged circularly. It also contains some amount of collagen and elastic tissues. This layer is thicker in arteries than in veins, allowing it to control the diameter of arteries, hence regulating the blood pressure and the blood flow.
- Tunica Intima: This is the innermost layer of the arterial wall, primarily composed of smooth endothelial cells. A single-layer simple squamous epithelial layer surrounded by a very thin layer of connective tissue with elastic fiber forms this layer.
Arteries arise from the left ventricle of the heart as a single main and largest artery called the aorta. The aorta is divided into four sections – ascending aorta, aortic arch, thoracic aorta, and abdominal aorta. From each section, different arteries, called the major arteries, arise. These major arteries branch repeatedly to form a network of systemic arteries that supply blood to all organs and tissues of the body.
The arteries become finer and finer as they branch out, and finally become arterioles; the finer arteries that supply to tissues. These arterioles further become smaller and are connected to capillaries to supply blood to every cell of the body.
Function of Arteries
Arteries carry blood away from the heart and to all body organs and tissues. Their thick muscular walls facilitate this function, enabling blood to be pumped under high pressure around the body. All arteries carry oxygenated blood except for the pulmonary arteries, which carry deoxygenated blood from the right ventricle to the lungs for oxygenation.
Veins
Veins are a vital part of the circulatory system, responsible for returning deoxygenated blood from various parts of the body back to the heart.
Structure of Veins
- Tunica Externa (Adventitia): This is the outermost layer, primarily made of connective tissues mainly with collagen fibers providing physical strength and elasticity to the veins.
- Tunica Media: This is the middle layer composed of connective tissue with elastic fibers and transverse layers of muscle fibers. The smooth muscle cells present in this layer help to regulate the diameter of veins.
- Tunica Intima: This is the innermost smooth layer made from endothelial cells providing a smooth surface for easy flow of the blood inside the veins.
Veins are thin-walled valves containing blood vessels. They have considerably lesser amounts of smooth muscles making them thinner than the walls of the arteries1. This thinner wall makes the veins more flexible and allows the veins to hold nearly 70% of total blood at any time.
Veins start as small finer tubules of about 8 to 100 μm in diameter, called the venules. The veins that are connected directly to the capillaries are called the post – capillary venules. Several venules merge forming a smaller vein. Different small veins unite forming larger veins that finally connect to form two major veins called the vena cava; the superior vena cava and the inferior vena cava. The vena cava drains the deoxygenated blood back into the heart at the right atrium.
Function of Veins
Veins collect the deoxygenated blood from every tissue and organ of our body and transport it back to the heart for reoxygenation and re-circulation. The veins carry the blood at very low pressure so they are equipped with venous valves that keep the blood flowing towards the heart by checking the backflow.
Capillaries
Capillaries are the smallest and most abundant blood vessels in the body, forming a network that connects arterioles to venules.
Structure of Capillaries: Capillaries are extremely thin, measuring approximately 5 micrometers in diameter. They are so small that red blood cells need to flow through them single file. The walls of capillaries are composed of only two layers of cells surrounded by a layer of protein called the basement membrane.
Types of Capillaries
There are three types of capillaries, each with a slightly different structure that allows it to function in a unique way,
- Continuous Capillaries: These are the most common types of capillaries. They contain small gaps in between their endothelial cells that allow for things like gases, water, sugar (glucose), and some hormones to pass through.
- Fenestrated Capillaries: Fenestrated capillaries are “leakier” than continuous capillaries. They contain small pores, in addition to small gaps between cells, in their walls that allow for the exchange of larger molecules.
- Sinusoidal Capillaries: Sinusoidal capillaries have large open pores that blood cells can pass through so they can be filtered and have defective cells removed.
Function of Capillaries: Capillaries connect the arterial system to the venous system. The exchange of oxygen, nutrients, and waste between your blood and tissues also happens in your capillaries. This happens through two processes: Passive diffusion and Pinocytosis.
Conduction system of heart
The conduction system of the heart is a network of specialized cardiac muscle cells that initiate and transmit the electrical impulses responsible for the coordinated contractions of each cardiac cycle.
Elements of the Conduction System: The conduction system comprises the following structures in order;
- Sinoatrial (SA) Node: Located in the upper wall of the right atrium, the SA node is a collection of specialized cells (pacemaker cells) that can spontaneously generate electrical impulses. The SA node is the primary impulse initiator and regulator in a healthy heart, making it the physiological pacemaker of the heart.
- Internodal and Interatrial Conduction Pathways: These pathways conduct impulses to the left atrium.
- Atrioventricular (AV) Node: Located within the atrioventricular septum, near the opening of the coronary sinus, the AV node acts to delay the impulses by approximately 120ms, to ensure the atria have enough time to fully eject blood into the ventricles before ventricular systole.
- Atrioventricular (AV) Bundle (Bundle of His): This bundle transmits the electrical impulse from the AV node to the Purkinje fibers of the ventricles.
- Right and Left Bundle Branches: These branches carry the impulses down the interventricular septum.
- Purkinje Fibers: These fibers spread the wave impulses along the ventricles, causing them to contract.
Heartbeat
A heartbeat is a two-part pumping action that takes about a second. Each time the chambers contract or relax, a thumping sound is produced. This is what is known as the heartbeat. A single heartbeat denotes that a complete cycle of pumping blood is finished.
The following sequence of electrical events occurs during one full contraction of the heart muscle:
- An excitation signal (an action potential) is created by the sinoatrial (SA) node.
- The wave of excitation spreads across the atria, causing them to contract.
- Upon reaching the atrioventricular (AV) node, the signal is delayed.
- It is then conducted into the bundle of His, down the interventricular septum.
- The bundle of His and the Purkinje fibers spread the wave impulses along the ventricles, causing them to contract.
Regulation by autonomic nervous system
The autonomic nervous system (ANS) plays a crucial role in regulating the heart’s conduction system. It influences most heart functions by affecting the sinoatrial (SA) node, atrioventricular (AV) node, myocardium, and small and large vessel walls. The ANS is divided into two main branches: the sympathetic and parasympathetic systems. These two systems have opposing effects on the heart:
Sympathetic System: This system carries an excitatory effect on heart functions. It increases the rate of SA node activity, thus increasing the heart rate and the force of heart contractions. This is particularly important during times of stress or exercise when the body requires more oxygen.
Parasympathetic System: Conversely, the parasympathetic system has inhibitory effects on heart functions. It decreases the rate of SA node activity, thus slowing down the heart rate. This is particularly important during times of rest and digestion.
The brain sends signals through the ANS to the heart’s electrical system. That system activates, sending an electrical pulse through the heart muscle. This is how the ANS helps regulate the heart rate and rhythm, adapting it to the body’s needs.
Cardiac output
Cardiac output (CO) is the volume of blood being pumped by a single ventricle of the heart per unit time, usually measured per minute. It is the product of the heart rate (HR), i.e., the number of heartbeats per minute (bpm), and the stroke volume (SV), which is the volume of blood pumped from the left ventricle per beat. The formula for cardiac output is:
CO=HR×SV
For a healthy individual weighing 70 kg, the cardiac output at rest averages about 5 L/min; assuming a heart rate of 70 beats/min, the stroke volume would be approximately 70 mL. Cardiac output is an important component of how efficiently the heart can meet the body’s demands for the maintenance of adequate tissue perfusion.
Cardiac Cycle
The cardiac cycle is the sequence of events that occurs in a complete heartbeat, from the beginning of one heartbeat to the beginning of the next. It consists of two main phases: diastole and systole.
- Diastole: During this phase, the heart muscle relaxes and the chambers fill with blood. This phase includes atrial diastole (when the atria are filling with blood) and ventricular diastole (when the ventricles are filling with blood).
- Systole: This phase involves the contraction of the heart muscle and the pumping of blood. It includes atrial systole (when the atria contract to push blood into the ventricles) and ventricular systole (when the ventricles contract to push blood out of the heart).
The cardiac cycle starts with both the atria and ventricles in diastole, the atria contract (atrial systole), and then the ventricles contract (ventricular systole). The cycle then repeats. Each cardiac cycle lasts about 0.8 seconds, with the heart beating about 70 to 75 times per minute.
Regulation of blood pressure
The regulation of blood pressure is a complex process that involves several mechanisms within the cardiovascular system.
Baroreceptor Reflex: The baroreceptor reflex is a neurally-mediated reflex that regulates blood pressure in the short term. This reflex is crucial for maintaining blood pressure throughout the day, and in its absence, even a slight change in posture could lead to significant changes in blood pressure. There are mechanoreceptors known as baroreceptors located in the aortic arch and carotid sinus, which constantly monitor the mean arterial blood pressure and pulse pressure.
When blood pressure increases, there is increased baroreceptor activity, increasing the firing rate in the associated afferent neurons, carrying this information to the cardiovascular center in the medulla. In response to this, the parasympathetic nervous system (PSNS) activity increases and the sympathetic nervous system (SNS) activity decreases. The net effect is reduced heart rate and systemic vasodilatation, collectively reducing mean arterial blood pressure.
Conversely, when blood pressure decreases, there is less baroreceptor activation meaning the impulse rate of the afferent fibers decreases, causing the cardiovascular center to increase SNS outflow and decrease PSNS outflow. The net effect of this is increased cardiac contractility, increased heart rate and increased systemic vasoconstriction, causing an overall increase in blood pressure.
Autonomic Nervous System: The autonomic nervous system (ANS) plays a crucial role in the regulation of blood pressure. The ANS, which includes the sympathetic and parasympathetic nervous systems, controls the heart rate, the force of the heart’s contractions, and the diameter of blood vessels.
The sympathetic nervous system increases heart rate and constricts blood vessels, thereby increasing blood pressure. On the other hand, the parasympathetic nervous system decreases heart rate, which in turn decreases blood pressure.
Renal Regulation: The kidneys also play a vital role in long-term regulation of blood pressure by controlling blood volume. When blood pressure is high, the kidneys increase urine production to reduce blood volume and lower blood pressure. Conversely, when blood pressure is low, the kidneys decrease urine production to increase blood volume and raise blood pressure.
Pulse
A pulse is the tactile arterial palpation of the cardiac cycle, also known as the heartbeat. It represents the rhythmic contraction and dilation of the arteries resulting from the beating of the heart. As the heart pumps blood into the arteries, the arteries expand and contract along with the flow of the blood. The pulse is thus the rate at which the heart beats.
You can measure a pulse by applying firm fingertip pressure to the skin at sites where the arteries travel near the skin’s surface. It is more evident when surrounding muscles are relaxed3. Common pulse points include the radial artery in the wrist and the carotid artery in the neck.
In most cases, three fingers are used to take the radial pulse measurement. The finger that is closest to the heart is used to occlude the pulse pressure. The middle-most finger is used to get a rough estimate of the blood pressure, and the finger that is most distal (typically, the ring finger) to the heart is used to void the effect of the ulnar pulse because the palmar arches connect the two arteries (superficial and deep).
The study of the pulse is known as sphygmology. A normal resting heart rate (when not exercising) for people age 15 and up is 60 to 100 beats per minute (bpm). However, your heart rate may vary slightly from the norm due to several factors, including regular exercise, a medical condition, stress, and use of some over-the-counter medications.
Electrocardiogram
An electrocardiogram (ECG or EKG) is a non-invasive test that monitors and records the electrical activity of your heart as it beats.
What is an Electrocardiogram (ECG)?
An ECG is a graphic record produced by an electrocardiograph that provides details about one’s heart rate and rhythm. It depicts if the heart has enlarged due to hypertension (high blood pressure) or evidence of a myocardial infarction previously (heart attack if any). ECGs from healthy hearts have a distinct, characteristic shape. Any inconsistency in the rhythm of the heart or damage to the heart muscle can alter the heart’s electrical activity thereby changing the shape on the ECG.
Why is an ECG Done?
An ECG is done to check the heartbeat. It shows how fast or how slow the heart is beating. ECG test results can help your care team diagnose irregular heartbeats, called arrhythmias, a previous heart attack, the cause of chest pain. For example, it may show signs of blocked or narrowed heart arteries. An ECG also may be done to learn how well a pacemaker and heart disease treatments are working.
How is an ECG Carried Out?
This test is usually done by trained technicians. Small metal disks (electrodes) which have wires that hook to an electrocardiograph machine are placed on the chest as you lie on the exam table. A lubricating gel is applied on the chest to help sound waves pass through the skin4. Selected sites are shaved, if necessary. During the test, you may be asked to remain motionless or hold your breath at times. The electrical activity is recorded as waves on a graph, with different patterns corresponding to each electrical phase of the heartbeat.
Risks: There is no risk of electric shock during an electrocardiogram. There are no side effects from the scan, although the lubricating gel may feel cold and you may experience some minor discomfort when the electrodes are removed from your skin at the end of the test.
Heart disorders
Heart disorders, also known as heart diseases, encompass a wide range of conditions that affect the heart’s structure and function.
- Coronary Artery Disease (CAD): CAD is the most common type of heart disease. It occurs when the coronary arteries, which supply blood to the heart muscle, become hardened and narrowed due to the buildup of plaque on the inner walls or lining of the arteries (atherosclerosis). This reduces the flow of oxygen-rich blood to the heart muscle, causing chest pain (angina) or a heart attack.
- Arrhythmias: Arrhythmias are problems with the rate or rhythm of the heartbeat. During an arrhythmia, the heart can beat too fast, too slow, or with an irregular rhythm. Some arrhythmias can cause problems such as fainting or stroke, or even sudden cardiac arrest.
- Congenital Heart Defects: These are heart problems that are present at birth. They can involve the walls of the heart, the valves of the heart, and the arteries and veins near the heart. Congenital heart defects can disrupt the normal flow of blood through the heart.
- Cardiomyopathy: This is a disease of the heart muscle that makes it harder for the heart to pump blood to the rest of the body. Cardiomyopathy can lead to heart failure.
- Valvular Heart Disease: Heart valve disease occurs when your heart’s valves do not work the way they should. The valves may not open enough to allow proper blood flow, or they may not close fully, allowing blood to leak backward.
- Endocarditis: This is an infection of the heart’s inner lining, usually involving the heart valves. It’s typically caused by bacteria entering the blood and settling in the heart.
Conclusion
The cardiovascular system is a complex and vital network that ensures the smooth functioning of our body. It comprises the heart, blood vessels (arteries, veins, and capillaries), and blood, which work together to deliver essential nutrients and oxygen to various organs and tissues, and remove waste products.
The heart’s conduction system, regulated by the autonomic nervous system, orchestrates the heart’s rhythm and rate. Tools like the electrocardiogram provide valuable insights into the heart’s electrical activity and help diagnose heart disorders. Despite its resilience, the cardiovascular system can be affected by various disorders, including coronary artery disease, arrhythmias, congenital heart defects, cardiomyopathy, valvular heart disease, and endocarditis.
Understanding the cardiovascular system’s structure, function, and potential disorders is crucial for maintaining good health and early detection and treatment of cardiovascular diseases. Regular check-ups and healthy lifestyle choices can help prevent many forms of heart disease.
For more regular updates you can visit our social media accounts,
Instagram: Follow us
Facebook: Follow us
WhatsApp: Join us
Telegram: Join us

1 thought on “Cardiovascular System”