Reproductive system
The human reproductive system is a complex and intricate network of organs and structures responsible for perpetuating our species. It encompasses both male and female components, each playing a vital role in the creation of new life. From the production of gametes (sperm and eggs) to the nurturing of a developing fetus, this system is a testament to the marvels of biology.
Male reproductive system
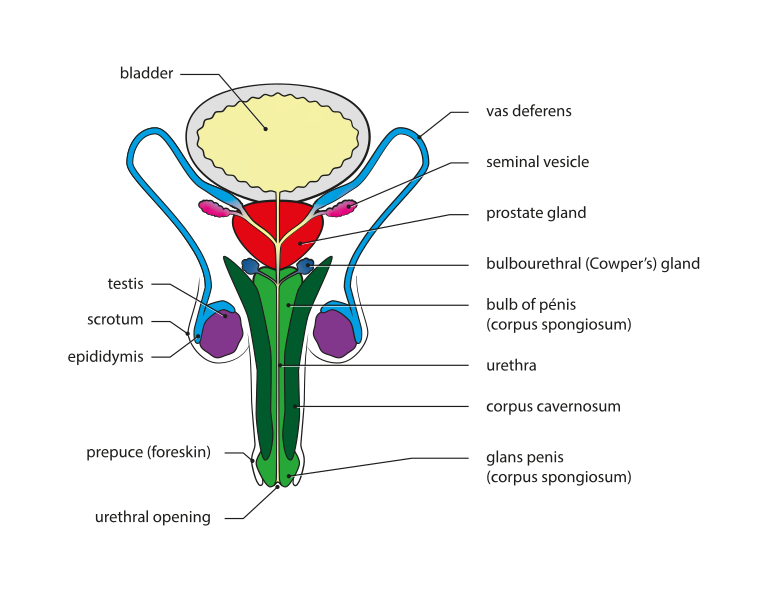
The male reproductive system is a complex network of organs that work together to produce, store and transport sperm, as well as secrete hormones that regulate male sexual function and development.
External Genitals
- Scrotum: A sac-like pouch of skin that hangs behind the penis. The scrotum keeps the testes cooler than the rest of the body, which is necessary for sperm production. The rugae, the wrinkled appearance of the scrotum, allows for expansion as the testes change temperature.
- Testes: The paired, oval-shaped testes are the male gonads, responsible for producing sperm and testosterone, the primary male sex hormone. Each testis is divided into hundreds of tiny compartments called seminiferous tubules, where sperm production (spermatogenesis) occurs.
- Penis: The cylindrical-shaped organ for sexual intercourse and urination. The penis consists of three columns of erectile tissue that fill with blood during arousal to cause an erection. The urethra, a tube that carries both urine and semen, runs along the underside of the penis. The glans penis, the bulbous head of the penis, is covered in loose skin called the foreskin.
Internal Genitals
- Epididymis: A coiled tube resting on the top of each testis. The epididymis stores and matures sperm cells after they leave the seminiferous tubules. Sperm can remain viable in the epididymis for several weeks.
- Vas deferens: A muscular tube that carries mature sperm cells from the epididymis up into the abdomen. The vas deferens joins with the seminal vesicle on each side to form the ejaculatory duct.
- Seminal vesicles: Two sac-like glands located near the base of the bladder. The seminal vesicles produce a thick, fructose-rich fluid that nourishes and protects sperm and makes up the bulk of semen.
- Prostate gland: A walnut-shaped gland that surrounds the urethra just below the bladder. The prostate gland produces a milky fluid that helps to liquefy semen and neutralize vaginal acidity, aiding sperm motility.
- Bulbourethral glands (Cowper’s glands): Two pea-sized glands located on either side of the urethra below the prostate. The bulbourethral glands produce a clear, alkaline fluid that lubricates the urethra and helps to neutralize any residual urine before ejaculation.
- Urethra: A tube that carries urine from the bladder out of the body and semen during ejaculation. The urethra passes through the penis and joins with the ejaculatory duct to form a single passage.
Functions of the male reproductive system
Sperm Production and Transport
- The male reproductive system is responsible for producing, maintaining, and transporting sperm cells (also known as spermatozoa) and semen.
- Sperm cells are the male reproductive cells essential for fertilization.
- Semen is the protective fluid that surrounds sperm and provides nutrients and mobility.
Discharge of Sperm
- During sexual intercourse, the male reproductive system facilitates the discharge of sperm into the female reproductive tract.
- This process allows sperm to reach the egg for fertilization.
Hormone Production
- The male reproductive system produces and secretes male sex hormones.
- The primary hormone is testosterone, which plays a crucial role in various aspects of male development, including muscle mass, bone density, fat distribution, and libido.
Specific Organs and Their Functions
- Testes: These are the male gonads and are responsible for sperm production.
- Epididymis: Sperm mature and gain motility in the epididymis.
- Vas Deferens: Tubes that transport sperm from the epididymis to the urethra.
- Prostate Gland: Produces seminal fluid that nourishes and protects sperm.
- Seminal Vesicles and Bulbourethral Glands: Contribute additional components to semen.
- Penis: The male organ for sexual intercourse.
Hormonal Regulation
- Hormones such as follicle-stimulating hormone (FSH) and luteinizing hormone (LH) play critical roles in spermatogenesis (sperm production).
- Testosterone, produced by the testes, influences male secondary sexual characteristics.
Female reproductive system
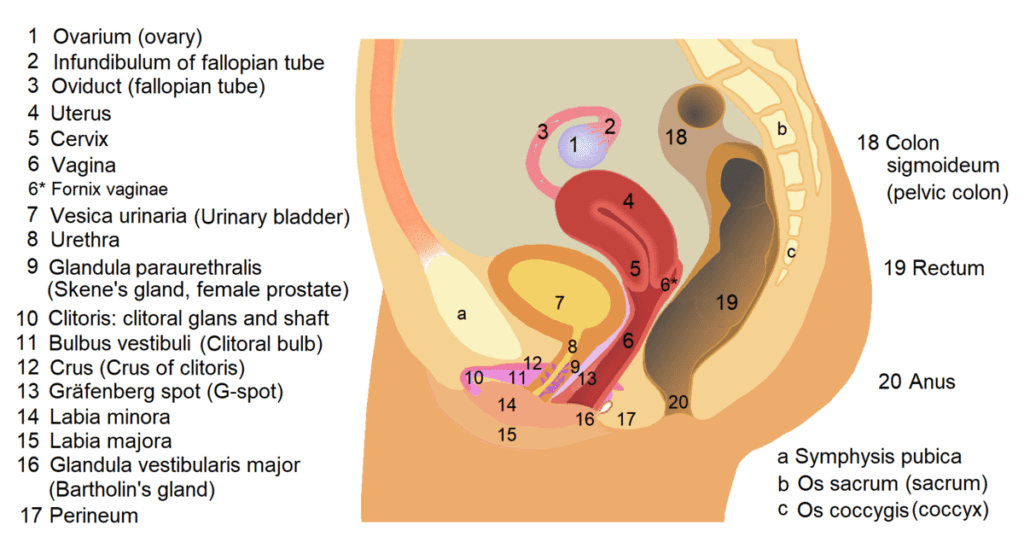
The female reproductive system is an intricate network of organs responsible for reproduction, menstruation, and hormone production.
Internal Organs
- Ovaries: These two oval-shaped glands, located on either side of the uterus in the lower abdomen, are the female gonads. The ovaries have two main functions:
Egg production (oogenesis): Each ovary contains follicles, which house immature eggs (oocytes). During a monthly cycle, one follicle matures and releases a mature egg (ovulation) through a process controlled by hormones.
Hormone production: The ovaries produce estrogen and progesterone, essential hormones for regulating the menstrual cycle, pregnancy, and development of female sexual characteristics.
- Fallopian tubes (uterine tubes): These slender tubes are located on either side of the uterus and connect the ovaries to the uterus. The fimbriae, finger-like projections at the end of each fallopian tube, help capture the released egg from the ovary. Fertilization, the fusion of sperm and egg, typically occurs in the fallopian tubes.
- Uterus: This pear-shaped, hollow organ located in the center of the lower abdomen is the site where a fertilized egg implants and grows during pregnancy. The muscular walls of the uterus allow for expansion during pregnancy and contraction during childbirth. The uterus has three main layers:
Myometrium: The thick, muscular middle layer responsible for contractions.
Endometrium: The inner lining of the uterus that thickens and sheds during menstruation if pregnancy doesn’t occur.
Perimetrium: The thin outer layer that connects the uterus to surrounding structures.
- Cervix: The lower, narrow end of the uterus that projects into the vagina. The cervix acts as a gateway between the vagina and the uterus. It produces mucus that changes consistency throughout the menstrual cycle, affecting sperm passage. The opening of the cervix (os) dilates during childbirth to allow the baby to pass through.
- Vagina: This muscular, elastic canal connects the cervix to the external opening of the body.
External Genitals (Vulva)
- Mons pubis: The fleshy pad covered with pubic hair located over the pubic bone.
- Labia majora: The larger, outer folds of skin that protect the vulva.
- Labia minora: The smaller, inner folds of skin that surround the opening of the vagina and the clitoris.
- Clitoris: A small, highly sensitive erectile tissue that plays a role in sexual pleasure.
- Vestibule: The space between the labia minora that contains the opening of the vagina, urethra (urinary opening), and openings of the Skene’s glands and Bartholin’s glands.
- Bartholin’s glands: Two glands located on either side of the vaginal opening that produce mucus for lubrication during sexual intercourse.
- Skene’s glands: Tiny glands located on either side of the urethra that also produce mucus for lubrication.
Functions of the female reproductive system
Egg Production (Oogenesis)
- The ovaries are the primary organs responsible for producing eggs (also known as ova).
- During each menstrual cycle, an egg matures within a fluid-filled sac called a follicle.
- Once released during ovulation, the egg enters the fallopian tube where it awaits fertilization by sperm.
Hormone Secretion: The female reproductive system produces essential hormones:
- Estrogen: Regulates the menstrual cycle, influences secondary sexual characteristics, and maintains bone health.
- Progesterone: Prepares the uterus for pregnancy and supports early pregnancy.
- These hormones play a crucial role in fertility, mood regulation, and overall health.
Uterus (Womb)
- The uterus provides a nurturing environment for a developing embryo.
- If fertilization occurs, the embryo implants into the uterine lining.
- During pregnancy, the uterus expands to accommodate the growing fetus.
Menstruation
- The uterus sheds its inner lining (endometrium) during menstruation if fertilization doesn’t occur.
- This cyclic process allows the body to prepare for potential pregnancy.
Childbirth
- The uterus contracts during labor to expel the baby through the vaginal opening.
- The cervix (lower part of the uterus) dilates to allow passage.
Breastfeeding
- After childbirth, the female reproductive system supports breastfeeding.
- The mammary glands produce milk to nourish the newborn.
Sex hormones
Sex hormones, also known as sex steroids, are chemical messengers produced by the gonads (testes in males and ovaries in females) and adrenal glands. They play a crucial role in several functions, most notably:
- Sexual development and reproduction: Sex hormones are responsible for the development of secondary sexual characteristics, such as breast development, body hair growth, and deepening of the voice in puberty. They also regulate the menstrual cycle in females and sperm production in males.
- Overall health and well-being: Sex hormones influence a wide range of bodily functions beyond reproduction. They impact bone density, muscle mass, mood, cognitive function, and metabolism.
There are three main categories of sex hormones:
Androgens: Often referred to as “male sex hormones,” the primary androgen is testosterone. However, androgens are present in both males and females, although at different levels. Testosterone is responsible for male sexual development, including muscle and bone growth, facial and body hair growth, and sperm production. In females, androgens play a role in bone health, sex drive, and fat distribution.
Estrogens: Primarily produced in the ovaries, estrogens are essential for female sexual development and function. They stimulate breast development, regulate the menstrual cycle, and influence bone health. Estrogens are also present in males in small amounts and contribute to sperm production.
Progestogens: The main progestogen in humans is progesterone, primarily produced by the ovaries after ovulation. Progesterone prepares the lining of the uterus (endometrium) for pregnancy and helps maintain it during pregnancy. It also plays a role in regulating the menstrual cycle and breast development.
Here’s a deeper dive into each sex hormone and its functions:
Testosterone
Production: Primarily produced in the testes by Leydig cells, with a small amount from the adrenal glands.
Functions in Males:
- Development and maintenance of male sexual organs and secondary sexual characteristics (muscles, facial and body hair, deepening voice).
- Sperm production.
- Bone and muscle growth.
- Sex drive (libido).
- Red blood cell production.
- Mood regulation.
Functions in Females:
- Sex drive (libido).
- Bone health.
- Muscle mass.
- Fat distribution.
Estrogens
Production: Primarily produced in the follicles of the ovaries, with a small amount from the adrenal glands and fat tissue.
Functions in Females:
- Development and maintenance of female sexual organs and secondary sexual characteristics (breasts, wider hips).
- Regulation of the menstrual cycle.
- Thickening of the endometrium (uterine lining) in preparation for pregnancy.
- Bone health.
- Mood regulation.
Functions in Males:
- Sperm production (in low amounts).
Progesterone
Production: Primarily produced by the corpus luteum in the ovary after ovulation, with a small amount from the adrenal glands and placenta during pregnancy.
Functions
- Preparing and maintaining the endometrium for pregnancy.
- Regulating the menstrual cycle.
- Breast development during pregnancy.
- Suppressing ovulation during pregnancy.
Hormonal Balance
Sex hormones work in a delicate balance, influencing and being influenced by each other. The hypothalamus and pituitary gland in the brain work together to regulate the production of sex hormones. Throughout life, sex hormone levels fluctuate naturally, particularly during puberty, the menstrual cycle, pregnancy, and menopause.
Imbalances in sex hormones can lead to various health problems in both males and females, such as infertility, irregular periods, osteoporosis, and decreased sex drive.
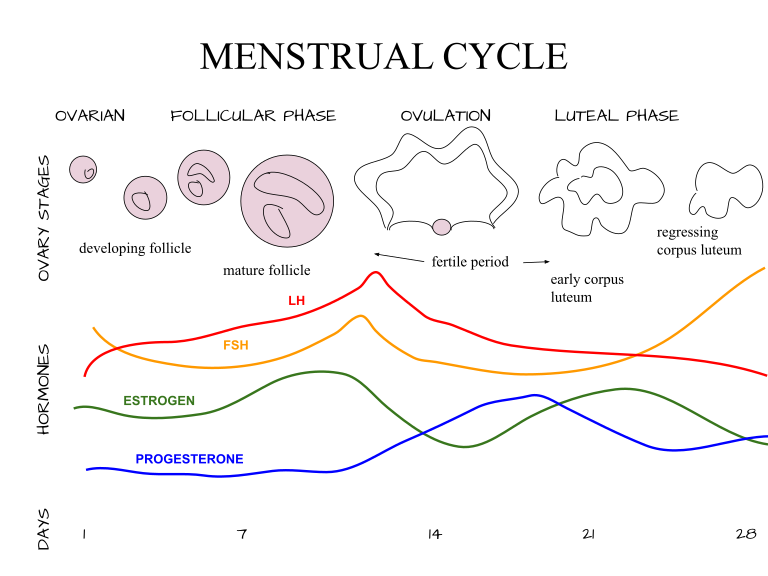
Menstrual cycle
- The menstrual cycle is a complex physiological process that occurs in females of reproductive age.
- It involves the cyclical shedding of the endometrium (the lining of the uterus).
- This process is regulated by intricate interactions between hormones from the hypothalamus, pituitary gland, ovaries, and uterus.
The Players
- Ovaries: These two bean-shaped organs produce eggs and sex hormones, primarily estrogen and progesterone.
- Endometrium: The inner lining of the uterus that thickens and undergoes changes throughout the cycle in preparation for a potential pregnancy.
- Hypothalamus and Pituitary Gland: These structures in the brain act as the control center, regulating hormone production in the ovaries.
The Phases
The menstrual cycle can be broken down into four main phases, each characterized by hormonal changes and specific events in the uterus:
Menstruation (Day 1 – 5)
- This is the period of bleeding you experience.
- Progesterone and estrogen levels have dropped significantly.
- The endometrium, no longer supported by hormones, breaks down and sheds along with blood vessels and tissue.
- The average blood loss is 30-80 ml, but it can vary.
- This phase typically lasts 3-5 days.
Follicular Phase (Day 6 – 14)
- The focus shifts to egg development.
- Follicle Stimulating Hormone (FSH) rises from the pituitary gland.
- FSH stimulates the ovaries to develop multiple follicles, each containing an immature egg.
- One dominant follicle emerges, while others regress.
- Estrogen levels rise steadily from the developing follicles.
- Estrogen stimulates the growth and thickening of the endometrium in preparation for a possible pregnancy.
Ovulation (Day 14 – 16)
- A surge in Luteinizing Hormone (LH) from the pituitary gland triggers ovulation.
- The dominant follicle ruptures, releasing a mature egg (ovum) into the fallopian tube.
- Estrogen levels peak just before ovulation.
Luteal Phase (Day 17 – 28)
- The empty follicle transforms into the corpus luteum, which produces progesterone.
- Progesterone prepares the endometrium to receive a fertilized egg by increasing blood flow and creating a more receptive lining.
- If fertilization doesn’t occur, the corpus luteum degenerates, leading to a drop in progesterone.
- The decline in progesterone triggers the breakdown of the endometrium, initiating menstruation (Day 1).
Regulation and Factors Affecting the Cycle
- The hypothalamus and pituitary gland in the brain control hormone production through a feedback loop.
- Changes in estrogen and progesterone levels send signals back to the brain, regulating their release.
- Stress, weight fluctuations, illness, certain medications, and travel can disrupt the menstrual cycle.
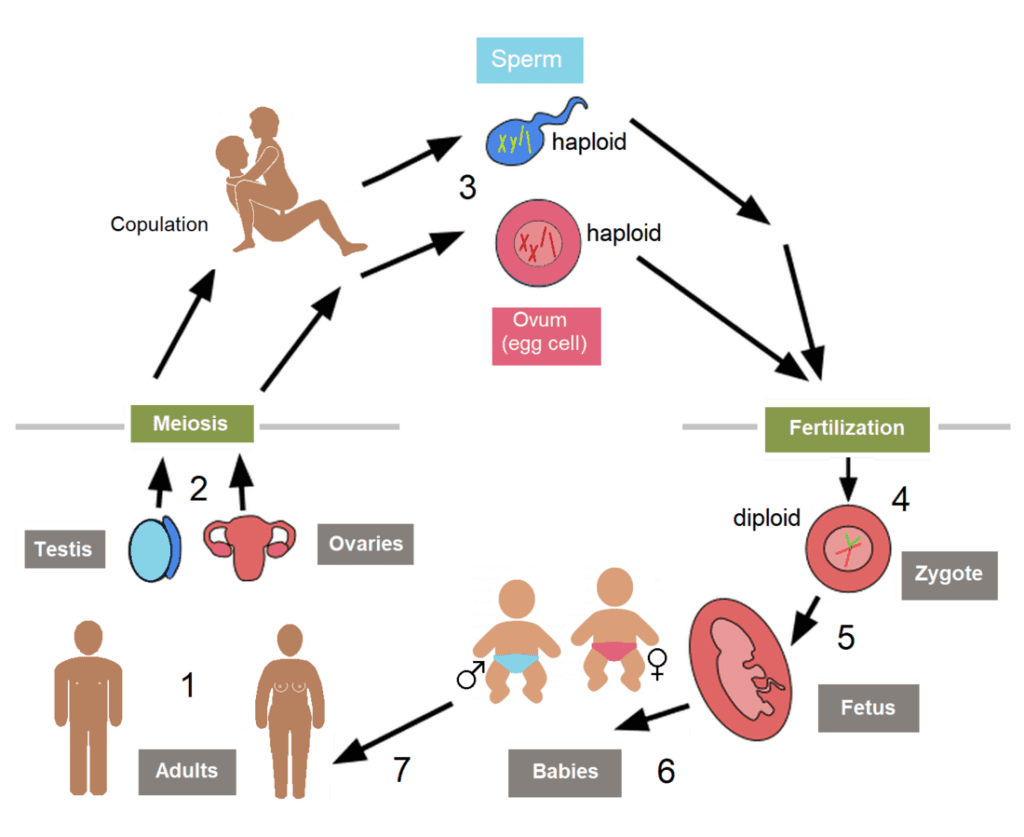
Physiology of fertilisation
Fertilization, the union of sperm and egg, is the crucial first step in human reproduction. It’s a complex dance of cellular interactions orchestrated by specific physiological events.
The Stage
Location: Fertilization typically occurs in the ampulla, the distal section of the fallopian tube closest to the ovary.
Players
- Sperm: The male gamete, containing half the genetic information (23 chromosomes).
- Egg (Oocyte): The female gamete, containing the other half of the genetic information (23 chromosomes).
The Act: The journey to fertilization involves several key steps:
- Sperm Transport: Millions of sperm are deposited in the vagina during sexual intercourse. They travel through the cervix, uterus, and eventually reach the fallopian tubes. This journey can take several hours.
- Sperm Capacitation: As sperm travel through the female reproductive tract, they undergo a process called capacitation. This modifies the sperm’s membrane, allowing them to bind to the zona pellucida, the protective layer surrounding the egg.
- The Acrosomal Reaction: Upon binding to the zona pellucida, the sperm releases enzymes from an organelle called the acrosome. These enzymes help the sperm penetrate the zona pellucida and reach the egg membrane.
- Fusion with the Egg: Only one sperm successfully fuses with the egg’s plasma membrane. This fusion triggers a reaction in the egg that prevents other sperm from entering (polyspermy block).
- Cortical Reaction: The egg undergoes a cortical reaction, releasing enzymes that modify the zona pellucida, making it impenetrable to other sperm.
- Nuclear Fusion: The head of the sperm, containing its nucleus with 23 chromosomes, enters the egg cytoplasm. The sperm’s nucleus and the egg’s nucleus (also containing 23 chromosomes) eventually fuse, forming a single nucleus with 46 chromosomes.
- Zygote Formation: With the fusion of nuclei, a fertilized egg, now called a zygote, is formed. The zygote contains the complete genetic information for a new organism.
Factors Affecting Fertilization
- Sperm Count and Motility: A healthy sperm count and good motility (movement) are essential for reaching and fertilizing the egg.
- Egg Quality: The egg’s health and maturity significantly impact fertilization success.
- Timing: The egg is only viable for about 24 hours after ovulation. Fertilization is most likely if sperm are present in the fallopian tubes during this window.
The Outcome
- If fertilization is successful, the zygote begins cell division and travels down the fallopian tube towards the uterus, eventually implanting in the endometrium (uterine lining) for further development.
- If fertilization doesn’t occur, the egg and unfertilized sperm are eventually broken down and absorbed by the body. The endometrium sheds during menstruation, marking the beginning of a new menstrual cycle.
Spermatogenesis
Spermatogenesis is the complex process by which sperm are produced in the male body, specifically within the testes. It’s a multi-stage process that involves the transformation of spermatogonia, which are immature germ cells, into mature spermatozoa (sperm cells).
Spermatocytogenesis: This is the first stage where spermatogonial stem cells undergo mitotic division near the basement membrane of the seminiferous tubules. This division results in two types of cells: Type A cells, which continue to serve as stem cells, and Type B cells, which differentiate into primary spermatocytes.
Meiosis: The primary spermatocytes enter meiosis I to form secondary spermatocytes, each with half the number of chromosomes (23 chromosomes). These secondary spermatocytes then undergo meiosis II to produce haploid spermatids.
Spermiogenesis: In this phase, spermatids undergo a series of morphological and structural changes to become spermatozoa. This includes the development of the acrosome, which is essential for egg penetration, and the formation of the flagellum for mobility.
Spermiation: Finally, the mature spermatozoa are released into the lumen of the seminiferous tubules and transported to the epididymis, where they gain motility and the ability to fertilize an egg.
The entire process of spermatogenesis takes about 74 days and is regulated by various hormones, including testosterone, follicle-stimulating hormone (FSH), and luteinizing hormone (LH). It’s a continuous process that starts at puberty and typically goes on throughout a man’s life.
Oogenesis
Certainly! Oogenesis is the process by which the female gametes, or ova (egg cells), are produced in the ovaries. It’s a complex and highly regulated process that involves several stages:
- Oogonia Formation: It begins during fetal development when a female fetus’s ovaries produce several million primordial germ cells called oogonia. These cells multiply by mitosis and form primary oocytes.
- Primary Oocytes: The primary oocytes begin the first meiotic division but get arrested in the prophase I stage. This arrest continues until the female reaches puberty.
- Resumption of Meiosis: At puberty, under the influence of hormones like Follicle-Stimulating Hormone (FSH), one primary oocyte each month completes the first meiotic division to form a secondary oocyte and a smaller cell called the first polar body.
- Secondary Oocyte: The secondary oocyte then starts the second meiotic division but gets arrested again at metaphase II. This oocyte is released from the ovary during ovulation.
- Completion of Meiosis: If the secondary oocyte is fertilized by a sperm, it completes the second meiotic division to form a mature ovum and a second polar body. If fertilization does not occur, the secondary oocyte degenerates1.
- Follicle Development: Parallel to oogenesis, follicle development occurs. Primary follicles containing primary oocytes develop into secondary follicles, which then become tertiary or Graafian follicles. These follicles have a fluid-filled cavity called the antrum.
- Ovulation: The Graafian follicle releases the secondary oocyte during ovulation. The remaining follicle cells transform into the corpus luteum, which produces progesterone, a hormone crucial for maintaining pregnancy.
The entire process of oogenesis is cyclical and coincides with the menstrual cycle. Unlike spermatogenesis, which produces millions of sperm daily, oogenesis results in the release of one secondary oocyte per month during a woman’s reproductive years.
Pregnancy and parturition
Pregnancy and parturition are two critical phases in the reproductive process.
Pregnancy
Pregnancy is the period during which a fertilized egg develops into a fetus inside a woman’s uterus. It lasts about 40 weeks, starting from the first day of the last menstrual period and is divided into three trimesters:
- First Trimester: The fertilized egg implants in the uterine wall and begins to grow. The major organs and structures of the baby start to form. This is also the most critical time for the baby’s development.
- Second Trimester: The baby’s bones become denser, and it starts to move in the womb. The mother may begin to feel the baby’s movements. The baby’s skin is covered with fine hair and a waxy coating.
- Third Trimester: The baby’s eyes can open and close, and it starts to store fat. The lungs are maturing and getting ready for breathing after birth. The baby moves into the birth position.
Parturition (Childbirth): Parturition is the process of giving birth to the baby. It involves three stages:
- Dilation: The first stage starts with the onset of labor and continues until the cervix is fully dilated to 10 centimeters. This stage is divided into the latent phase (cervix dilates from 0 to 4 cm) and the active phase (cervix dilates from 4 to 10 cm). The latent phase can take about six hours for a first-time mother and around five hours for subsequent births.
- Expulsion: The second stage begins when the cervix is fully dilated and continues until the birth of the baby. It includes the passive phase (the baby’s head moves down the vagina) and the active phase (the mother feels the need to push). This stage lasts about 45 minutes for a first-time mother and about 30 minutes for those who’ve had previous vaginal deliveries.
- Placental: The third stage starts after the birth of the baby and ends with the delivery of the placenta and membranes. If the doctor assists, this stage typically takes around five minutes. Without assistance, it can last around 30 minutes.
Complications can occur during any of these stages, such as fetal distress or nuchal cord (umbilical cord wrapped around the baby’s neck), which may necessitate medical interventions like cesarean delivery.
The process of parturition is regulated by hormones, including oxytocin, which induces uterine contractions necessary for the expulsion of the baby. After birth, the hormone also helps in reducing bleeding and facilitating the delivery of the placenta.
Conclusion
The human reproductive system is a marvel of biological engineering, intricately designed to ensure the continuation of our species. The male and female reproductive systems, though distinct in structure and function, work in concert to create new life. Spermatogenesis and oogenesis represent the cornerstone processes of gametogenesis, ensuring genetic diversity and the propagation of genetic material to future generations. Pregnancy and parturition epitomize the culmination of these processes, highlighting the body’s remarkable ability to nurture and bring forth new life. Understanding the complexities of the human reproductive system not only underscores the importance of reproductive health but also deepens our appreciation for the delicate balance of life itself.
For more regular updates you can visit our social media accounts,
Instagram: Follow us
Facebook: Follow us
WhatsApp: Join us
Telegram: Join us



One response to “Reproductive System”
[…] Reproductive system […]