Urinary System
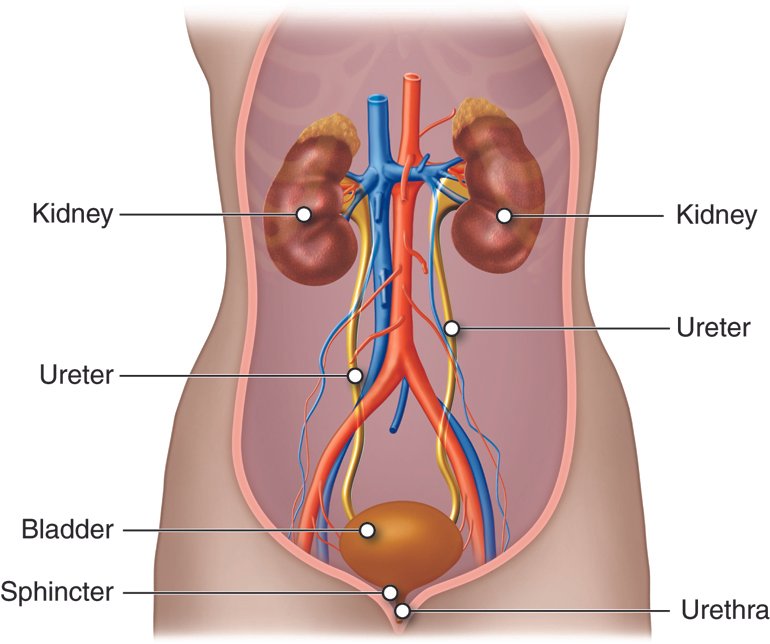
The urinary system, also known as the urinary tract, plays a crucial role in maintaining homeostasis within our bodies. It consists of several organs that work together to filter blood, eliminate waste products, and regulate fluid balance. Here are the key components of the urinary system:
- Kidneys: These remarkable bean-shaped organs are the stars of the show. You have two kidneys, located on either side of your back, just below the rib cage. Their primary function is to filter blood, removing waste products, excess water, and toxins. Each day, your kidneys filter an impressive 120 to 150 quarts (113.6 to 141.95 liters) of blood, producing about 1 to 2 quarts (0.95 to 1.95 liters) of urine.
- Ureters: These ducts connect the kidneys to the bladder. They transport urine from the kidneys to the bladder for storage.
- Bladder: The bladder is like a flexible reservoir that holds urine until you’re ready to release it. When it’s full, it sends signals to your brain, prompting you to visit the restroom.
- Urethra: This tube connects the bladder to the outside world. It allows urine to exit your body during urination.
Kidney
Anatomy of kidney
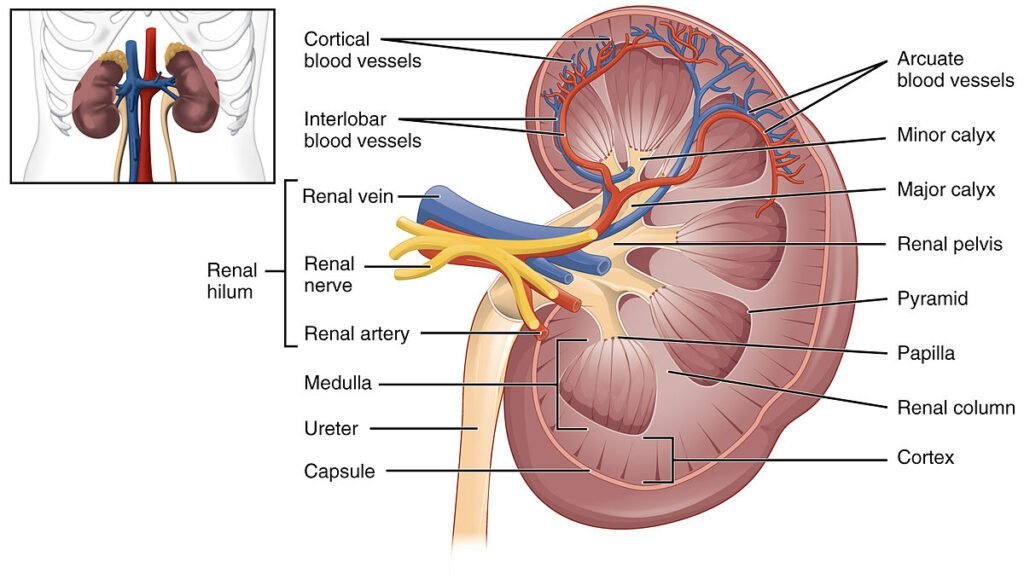
External Anatomy
- The kidneys are bilateral organs placed retroperitoneally in the upper left and right abdominal quadrants.
- Their shape resembles a bean, with the following features:
- Superior Pole: The upper end of the kidney.
- Inferior Pole: The lower end of the kidney.
- Major Convexity: The lateral side of the kidney.
- Minor Concavity: The medial side of the kidney.
- The kidneys are roughly the size of a closed fist, measuring about 10 to 12 centimeters long, 5 to 7 centimeters wide, and 3 to 5 centimeters thick.
- Each kidney is connected to the bladder through a ureter.
Internal Anatomy: Each kidney consists of several distinct regions;
- Renal Cortex: The outer layer where blood filtration occurs.
- Renal Medulla: The inner layer containing pyramid-shaped structures called renal pyramids.
- Renal Pelvis: A funnel-shaped area where urine collects before entering the ureter.
Nephron: The functional unit of the kidney, responsible for filtering blood and forming urine. Each kidney contains millions of nephrons.
Vasculature and Lymphatic Drainage
- Arteries: The renal artery, a branch of the abdominal aorta, supplies blood to the kidneys.
- Veins and Lymphatics: The renal vein drains blood from the kidneys into the inferior vena cava.
Innervation: The kidneys receive nerve supply from the renal plexus.
Functions of the Kidneys
Filtration and Waste Removal
- Your kidneys are the main organs of the urinary system.
- They filter blood to remove waste products and excess water.
- Healthy kidneys filter about a half cup of blood every minute, producing urine.
- This filtration process ensures that toxins, urea, and other waste materials are eliminated from your body.
Fluid Balance Regulation
- The kidneys play a crucial role in maintaining overall fluid balance.
- They regulate the amount of water in your body by adjusting urine production.
- When you’re dehydrated, the kidneys conserve water; when you’re well-hydrated, they excrete excess water as urine.
Electrolyte Balance
- Kidneys filter and regulate minerals (electrolytes) such as sodium, potassium, calcium, and phosphorus.
- Proper electrolyte balance is essential for nerve function, muscle contraction, and overall health.
Acid-Base Balance
- Kidneys help maintain the body’s pH level by excreting excess hydrogen ions (acid) or retaining bicarbonate ions (base).
- This balance is crucial for normal cellular function.
Hormone Production: Kidneys produce hormones that influence various bodily functions;
- Renin: Regulates blood pressure by affecting blood vessel constriction.
- Erythropoietin: Stimulates red blood cell production in the bone marrow.
- Calcitriol: Activates vitamin D, promoting calcium absorption for strong bones.
Blood Pressure Control
- By adjusting fluid volume and releasing renin, kidneys help regulate blood pressure.
- Renin activates the renin-angiotensin-aldosterone system, which affects blood vessel constriction and fluid balance.
Red Blood Cell Production
- Erythropoietin stimulates the bone marrow to produce red blood cells.
- Adequate red blood cells are essential for oxygen transport and overall health.
Bone Health
- Kidneys maintain calcium and phosphorus levels, crucial for bone strength.
- Calcitriol (activated vitamin D) enhances calcium absorption from the intestines.
Nephron
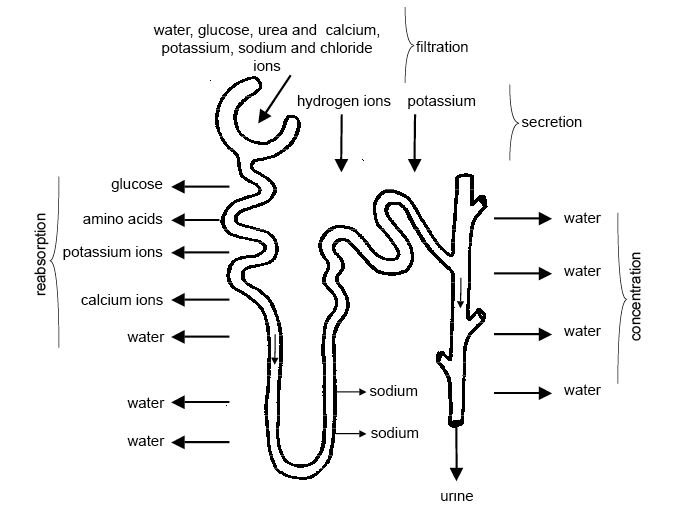
Renal Corpuscle: The renal corpuscle is the initial part of the nephron. It consists of two main components:
- Glomerulus: A tuft of capillaries where blood filtration occurs. The glomerulus is surrounded by Bowman’s capsule.
- Bowman’s Capsule: A cup-shaped structure that encloses the glomerulus.
- Blood flows into and away from the glomerulus through tiny arteries called arterioles.
- In the renal corpuscle, fluid filters out of the blood in the glomerulus and enters the nephron tubule.
Renal Tubule: The renal tubule extends from Bowman’s capsule. It consists of several segments:
- Proximal Tubule: Located immediately after Bowman’s capsule. Here, selective reabsorption of water and essential substances occurs.
- Loop of Henle: A U-shaped loop that extends into the medulla. It plays a crucial role in concentrating urine.
- Distal Tubule: Follows the loop of Henle. Further fine-tuning of electrolyte balance and pH occurs here.
- Collecting Duct: Collects urine from multiple nephrons and transports it toward the renal pelvis.
Location
- Renal corpuscles are located in the renal cortex.
- The tubular system extends into the renal medulla.
Nephron Function
Ultrafiltration
- Blood enters the glomerulus, and water, ions, and small molecules are filtered into Bowman’s capsule.
- This initial filtrate is called glomerular filtrate.
Selective Reabsorption
- As the filtrate moves through the tubules, essential substances (glucose, amino acids, ions) are reabsorbed back into the blood.
- Water is also reabsorbed, concentrating the filtrate.
Secretion
- Certain substances (e.g., hydrogen ions, drugs) are actively secreted into the tubules.
- This process helps regulate pH and eliminate waste products.
Urine Formation
- The final product is urine, which contains waste products and excess water.
- Urine travels through the collecting ducts to the renal pelvis and eventually exits the body through the ureters.
Ureters
Anatomy of the Ureters
Structure
- The ureters are bilateral, muscular, tubular structures.
- Each ureter is about 25 cm (approximately 12 inches) long.
- They emerge from the renal pelvis of each kidney and descend behind the abdominal cavity.
- As they approach the bladder, they narrow progressively, eventually opening into the bladder.
Lumen and Mucosal Layer
- The lumen (inner space) of each ureter is lined by a mucosal layer of urothelium (also known as transitional epithelium).
- This lining accommodates the increase in pressure that occurs when urine volume leaving the kidney rises.
- The multiple layers of smooth muscle throughout the ureteral wall allow it to handle this pressure without rupturing.
- Peristaltic motions initiated by pacemaker cells in the proximal renal pelvis propel urine along the ureters.
Muscular Layers: From a histological perspective, the ureter wall contains two main muscular layers;
- Longitudinal Layer: Runs along the length of the ureter.
- Circular Layer: Encircles the ureter.
In the lower segment of the ureters (proximal to the bladder), an additional longitudinal layer is present.
Functions of Ureter
- Muscles in the ureter walls continually tighten and relax, creating peristaltic waves.
- These waves force urine downward, away from the kidneys, toward the bladder.
- The ureters’ collapsible, S-shaped design allows them to adapt to changes in urine volume and pressure
Urinary bladder
The bladder is a vital part of your urinary system, responsible for storing urine before it leaves your body through the urethra.
Anatomy of the Bladder
Location
- The bladder is situated in the lower part of your abdomen (pelvis).
- It is held in place by ligaments that connect it to other organs and the hip bone.
- In males, it rests between the pubic bone (front) and the rectum (back).
- In females, it lies in front of the vagina and uterus.
Structure: The bladder has four main parts;
- Dome: The top-front part of the bladder, pointing toward the abdominal wall.
- Base: The bottom-back part (also called the fundus).
- Body: The area between the dome and the base.
- Neck: A narrow group of muscles connecting to the urethra.
Appearance
- When empty, the bladder is about the size and shape of a pear.
- It can stretch significantly, expanding up to 6 inches when full.
The bladder consists of three main layers:
- Urothelium: The inner lining that prevents urine leakage.
- Lamina propria (submucosa): A thin layer of connective tissue containing blood vessels and nerves.
- Muscularis propria: Smooth muscle fibers controlling urine flow.
Function of the Urinary Bladder
Urine Storage
- The primary function of the bladder is to hold urine.
- As your kidneys filter blood, waste products, salt, and water, urine accumulates in the bladder.
- When the bladder fills with approximately 200-350 mL of urine, nerves signal your brain that it’s time to use the restroom.
Urination
- When you need to pee, muscles in the bladder contract (tighten), and the sphincter muscles in the urethra relax.
- This coordinated action allows urine to flow out of your body through the urethra.
- Most people urinate about 950-1,900 mL (approximately two quarts) each day.
Urethra
The urethra is a hollow tube positioned between the urinary bladder and the external opening (urinary meatus). Its primary function is to carry urine stored in the bladder out of the body.
Length and Differences: Urethra length varies between males and females;
Male Urethra
- Approximately 15-20 cm long.
- Besides urine, it also transports semen (containing spermatozoa and sex gland secretions).
- Divided anatomically into three parts:
- Prostatic urethra: Begins at the bladder neck, passes through the prostate gland, and receives ejaculatory ducts and prostatic ducts.
- Membranous urethra: Passes through the pelvic floor and deep perineal pouch. Surrounded by the external urethral sphincter (voluntary control of micturition).
- Penile (bulbous) urethra: Passes through the penis bulb and corpus spongiosum, ending at the external urethral orifice (meatus).
Female Urethra
- Shorter (about 4 cm).
- Primarily involved in urine elimination.
Neurovascular Supply
Arterial supply to the male urethra:
- Prostatic urethra: Supplied by the inferior vesical artery (from the internal iliac artery).
- Membranous urethra: Supplied by the bulbourethral artery (branch of the internal pudendal artery).
- Penile urethra: Directly supplied by branches of the internal pudendal artery.
Nerve supply: Derived from the prostatic plexus (sympathetic, parasympathetic, and visceral afferent fibers).
Lymphatic Drainage
- Prostatic and membranous portions drain to the obturator and internal iliac nodes.
- Penile urethra drains to the deep and superficial inguinal nodes.
Functions of the Urinary System
The urinary system performs several essential functions:
- Excretion: It removes waste products from the body.
- Water Balance: It maintains the body’s water balance.
- Salt (Electrolyte) Balance: It regulates the concentration of salts (electrolytes) in the blood.
- Acid-Base (pH) Balance: It helps regulate the blood’s acid-base balance.
- Blood Volume Regulation: It plays a role in regulating blood volume.
- Blood Pressure Regulation: By releasing the enzyme renin, it helps regulate blood pressure.
- Red Blood Cell Production: It releases the hormone erythropoietin, stimulating red blood cell production.
- Vitamin D Activation: It converts vitamin D to its active form, calcitriol.
Physiology of urine formation
The process of urine formation involves several intricate steps within the nephrons of the kidneys. Here’s a breakdown of how it happens:
Glomerular Filtration
- Glomerular filtration occurs in the renal corpuscles (specifically, the glomerulus).
- Blood entering the kidney is filtered to form renal filtrate, which is a combination of blood plasma and waste products.
- The glomerulus acts as a filter, allowing small molecules (such as water, sodium, chloride, and bicarbonate) to pass through into the Bowman’s capsule.
- Larger molecules (such as proteins) remain in the blood.
Tubular Reabsorption
As the renal filtrate travels along the nephron tubules, specialized cells lining the tubules selectively reabsorb essential substances back into the bloodstream. These substances include:
- Water: Up to 99% of the water lost during filtration.
- Ions (Sodium, Potassium, Chloride): Vital for maintaining electrolyte balance.
- Glucose and Amino Acids: Reclaimed by tubule cells.
The goal is to prevent the loss of important molecules in the urine.
Tubular Secretion
- Tubular secretion mainly occurs in the proximal convoluted tubule (PCT) and distal convoluted tubule (DCT).
- Unfiltered substances (such as antibiotics, toxins, excess hydrogen ions, and potassium ions) are actively moved from the peritubular capillaries into the tubule lumen.
- These substances are destined to leave the body as components of urine.
Urine Formation
- The modified filtrate, after reabsorption and secretion, becomes urine.
- The collecting ducts further concentrate the urine by reabsorbing water.
- The final urine is then excreted through the ureters and stored in the bladder until elimination.
Micturition reflex
Bladder and Urethra
- The bladder is a hollow muscular organ that stores urine until it’s ready for elimination.
- The urethra is the tube that connects the bladder to the external environment, allowing urine to exit the body.
Detrusor Muscle
- The bladder walls are composed of smooth muscle called the detrusor muscle.
- When the bladder fills with urine, stretch receptors in the bladder wall are activated.
- These receptors send signals to the spinal cord and brain, indicating that the bladder is reaching its capacity.
Micturition Center
- The micturition center is located in the pons of the brainstem.
- It coordinates the micturition reflex and integrates sensory information from the bladder, spinal cord, and higher brain centers.
Parasympathetic Nervous System Activation
- As the bladder fills, parasympathetic nerves are activated.
- These nerves release the neurotransmitter acetylcholine, which binds to receptors on the detrusor muscle.
- Acetylcholine causes the detrusor muscle to contract, leading to increased pressure within the bladder.
Internal Urethral Sphincter Relaxation
- The internal urethral sphincter, a ring of smooth muscle at the bladder neck, is involuntarily controlled.
- When the bladder is full, stretch receptors signal the spinal cord, which inhibits the sympathetic nerves that normally keep the internal sphincter contracted.
- This inhibition allows the internal sphincter to relax, opening the passage between the bladder and the urethra.
Voluntary Control and External Urethral Sphincter
- The external urethral sphincter surrounds the urethra and is under conscious control.
- When you consciously decide to urinate, you voluntarily relax the external sphincter.
- This allows urine to flow from the bladder through the urethra and out of the body.
Coordination and Voiding
- When the micturition center receives signals that the bladder is full and external sphincter relaxation is appropriate (e.g., when you’re in a safe environment), it initiates voiding.
- The detrusor muscle contracts rhythmically, and the external sphincter relaxes, allowing urine to flow out of the body.
Role of kidney in Acid-Base balance
The kidneys play a crucial role in maintaining the delicate acid-base balance (pH) of our internal environment. Here’s how they achieve this:
Bicarbonate Reabsorption
- The kidneys reabsorb bicarbonate ions (HCO₃⁻) from the urine back into the bloodstream.
- Bicarbonate acts as a buffer, helping to neutralize excess acid (hydrogen ions, H⁺) in the blood.
- By reabsorbing bicarbonate, the kidneys prevent the blood from becoming too acidic.
Hydrogen Ion Excretion
- The kidneys excrete hydrogen ions (H⁺) into the urine.
- When blood becomes too acidic (due to factors like metabolism or diet), the kidneys increase the secretion of hydrogen ions.
- These hydrogen ions combine with bicarbonate in the urine, forming carbonic acid (H₂CO₃), which eventually breaks down into water and carbon dioxide.
Ammonium Buffer System
- The kidneys also play a role in the ammonium buffer system.
- When blood pH drops (becomes more acidic), the kidneys increase the excretion of ammonium ions (NH₄⁺) into the urine.
- Ammonium ions act as buffers, helping to neutralize excess acid.
Excretion of Excess Bicarbonate
- In cases of alkalosis (when blood becomes too basic), the kidneys excrete more bicarbonate into the urine.
- This helps reduce the alkalinity and maintain a balanced pH.
Long-Term Compensation
- While the lungs can adjust pH rapidly (within minutes), the kidneys provide long-term compensation.
- Renal mechanisms take hours to days to fully compensate for acid-base imbalances.
Role of RAS in kidney
The Renin-Angiotensin System (RAS), also known as the Renin-Angiotensin-Aldosterone System (RAAS), plays a critical role in regulating blood pressure, fluid and electrolyte balance, and systemic vascular resistance. This hormone system is especially important in the kidney’s function and overall cardiovascular health. Here are the key aspects of the RAS in the kidney:
Renin Production
- When renal blood flow decreases (due to factors like low blood volume or low blood pressure), specialized cells called juxtaglomerular cells in the kidneys release the enzyme renin.
- Renin converts the precursor protein angiotensinogen, released by the liver, into a decapeptide called angiotensin I.
Angiotensin-Converting Enzyme (ACE)
- Angiotensin I is subsequently converted to angiotensin II by the angiotensin-converting enzyme (ACE).
- ACE is primarily found on the surface of vascular endothelial cells, especially in the lungs.
Functions of Angiotensin II
- Vasoconstriction: Angiotensin II narrows blood vessels, leading to increased blood pressure.
- Aldosterone Stimulation: Angiotensin II stimulates the secretion of the hormone aldosterone from the adrenal cortex. Aldosterone causes the renal tubules to increase the reabsorption of sodium (Na⁺) and water into the blood. Simultaneously, it promotes the excretion of potassium (K⁺) to maintain electrolyte balance. These actions increase the volume of extracellular fluid, further raising blood pressure.
Blood Pressure Regulation
- If the RAS is abnormally active, blood pressure can become too high.
- Drugs like ACE inhibitors, angiotensin II receptor blockers (ARBs), and renin inhibitors interrupt different steps in this system to improve blood pressure.
- These medications are essential for controlling high blood pressure, heart failure, kidney failure, and the harmful effects of diabetes.
Disorders of kidney
Chronic Kidney Disease (CKD): CKD is a condition characterized by a gradual loss of kidney function over time.
Symptoms: Early stages may be asymptomatic. As the disease progresses, symptoms may include:
- Nausea
- Loss of appetite
- Fatigue
- Edema (swelling of feet and ankles)
- High blood pressure (hypertension)
- Increased urination, especially at night
- Decreased mental sharpness
- Sleep disturbances
- Blood in urine
- Protein in urine
- Erectile dysfunction in men
- Muscle twitching and cramps
- Persistent itching
- Chest pain (if fluid builds up around the lining of the heart)
- Shortness of breath (if fluid accumulates in the lungs)
Causes
- Diabetes (both type 1 and type 2)
- High blood pressure (hypertension)
- Glomerulonephritis (inflammation of the glomeruli)
- Polycystic kidney disease
- Autoimmune diseases (e.g., systemic lupus erythematosus)
- Vesicoureteral reflux (urine flowing back to the kidneys)
- Pyelonephritis (kidney infection)
- Interstitial nephritis (inflammation of the kidney tubules)
- Kidney stones, obstructions, or cancer
- Overuse of certain medications
- Drug abuse (heroin or cocaine)
Complications
- Fluid retention (swelling in arms and feet)
- Cardiovascular disease (affecting the heart and blood vessels)
- Imbalance in potassium levels (can be life-threatening)
- Decreased immune response
- Impaired central nervous system
- Pregnancy complications
- Complete loss of kidney function in late stages
Prevention
- Monitor and control blood sugar and blood pressure
- Avoid smoking
- Limit alcohol consumption
- Exercise regularly
- Maintain a healthy diet
- Control medication use
Treatment
- Manage symptoms and slow disease progression in early stages.
- Advanced stages may require dialysis or kidney transplant.
Acute Kidney Injury (AKI): AKI is a sudden and severe decline in kidney function.
Causes
- Dehydration
- Reduced blood flow to the kidneys (due to low blood pressure, heart failure, or shock)
- Kidney infections
- Medications (e.g., NSAIDs, certain antibiotics)
- Obstruction (e.g., kidney stones)
- Glomerulonephritis
- Hemolytic uremic syndrome (often caused by E. coli infection)
Symptoms
- Decreased urine output
- Swelling
- Fatigue
- Nausea
- Confusion
- Shortness of breath
Treatment
- Address the underlying cause
- Supportive care (fluids, electrolyte balance, and dialysis if necessary)
Kidney Stones: Hard deposits of minerals and salts that form in the kidneys.
Symptoms
- Severe pain (renal colic) in the back or side
- Pain radiating to the lower abdomen and groin
- Blood in urine
- Frequent urination
Treatment
- Pain management
- Increased fluid intake
- Medications to help pass the stone
- Surgical removal in severe cases
Polycystic Kidney Disease (PKD): A genetic disorder causing fluid-filled cysts to develop in the kidneys.
Symptoms
- Abdominal pain
- High blood pressure
- Blood in urine
- Kidney stones
Treatment
- Manage symptoms
- Blood pressure control
- Dialysis or kidney transplant in advanced cases
Conclusion
In conclusion, the urinary system is a remarkable orchestra of organs and processes that maintain our internal balance. From the kidneys’ intricate filtration to the bladder’s storage capacity, each component plays a vital role:
- Kidneys: These bean-shaped organs filter blood, remove waste products, and regulate fluid balance. They also produce hormones like erythropoietin and renin.
- Ureters: These ducts connect the kidneys to the bladder, ensuring urine transport.
- Bladder: The flexible reservoir stores urine until it’s time for elimination.
- Urethra: This tube connects the bladder to the external environment, allowing urine to exit the body.
The kidneys orchestrate fluid, electrolyte, and acid-base balance, ensuring our well-being. Whether it’s the intricate nephrons or the micturition reflex, the urinary system harmonizes our internal environment, keeping us in tune with life’s rhythm!
For more regular updates you can visit our social media accounts,
Instagram: Follow us
Facebook: Follow us
WhatsApp: Join us
Telegram: Join us

1 thought on “Urinary System”